The Key Quality Factors for PBMC Isolation
Having high-quality PBMCs for clinical research studies is vital to success, so it is essential to ensure that the isolation process is correct to achieve accurate and reliable research results

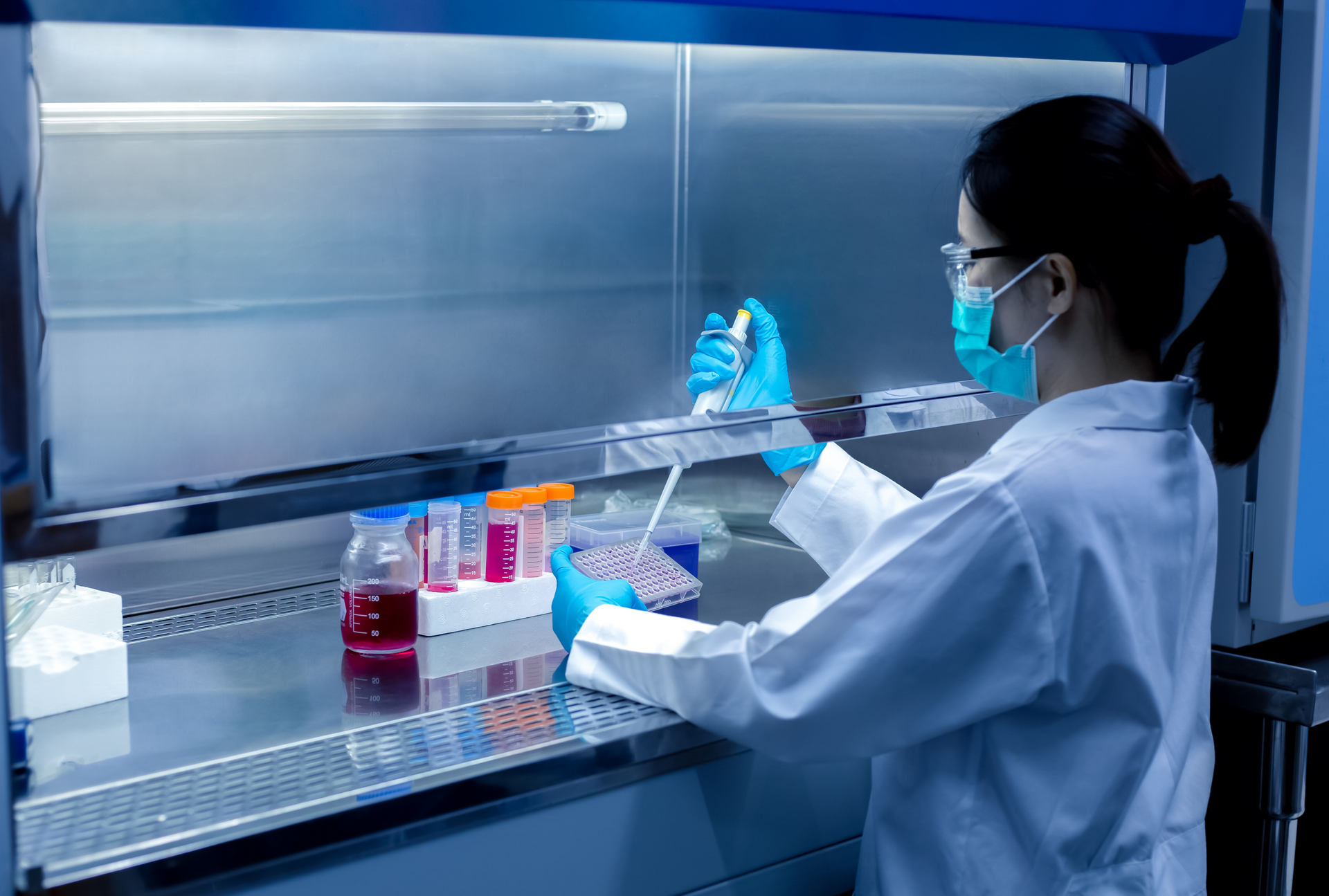
Isolating Peripheral Blood Mononuclear Cells or PBMCs is an essential process for any clinical research institution that works with blood samples. PBMCs are critical to various areas of research, including immunology, cancer, gene therapy, and infectious diseases. Having high-quality PBMCs for clinical research studies is vital to success, so it is essential to ensure that the isolation process is correct to achieve accurate and reliable research results. In this blog post, we will highlight the key quality factors that should be considered when isolating PBMCs.
Sample Collection
The PBMC isolation process begins with collecting the blood sample. The sample must be collected correctly to ensure the PBMC quality. Collection tubes must be coated with an anticoagulant to prevent the blood from clotting. Contamination can occur during the collection process due to poor hygiene or improper use of antiseptics. To avoid contamination, it is crucial to prepare the collection site correctly, follow hygienic practices, and sterilize equipment used in sample collection.
Sample Processing
The process of isolating PBMCs requires blood separation by centrifugation. During this process, the sample must be handled and processed carefully to prevent any damage to the cells. Although the centrifugation process is essential for isolating PBMCs, it can also cause cellular damage. The centrifuge must be correctly calibrated, and the centrifugation time and speed must be precise to ensure that the desired cells are separated and undamaged.
Cell Counting
Counting the PBMCs accurately is a critical quality factor, as it determines the concentration of PBMCs that are needed for different research studies. An accurate cell count also helps ensure the consistency of experiments across different batches of PBMCs. Based on the standard operating procedure, automated cell counters or manual counting are utilized to count the cell accurately.
Cell Viability
One of the most critical quality factors for PBMC isolation is cell viability. Cell viability refers to the percentage of live cells in a sample. The higher the percentage of live cells, the more accurate and reliable the results of the research. Dead cells may not respond to different treatments or stimuli, leading to inaccurate research results. Viability can be assessed using Trypan Blue staining or a flow cytometry analysis. It is essential to maintain cell viability during the isolation, processing, and storage of PBMC samples.
Cryopreservation
Cryopreservation, the process of freezing cells, is commonly used to store PBMCs. The frozen PBMCs can be stored for future research experiments, saving time and effort on repeating the isolation process. However, the quality of frozen PBMC samples can deteriorate over time, leading to fewer viable cells when thawed. Careful attention must be given to the freezing and thawing process to maintain high-quality PBMCs for research.
In conclusion, PBMC isolation is a crucial process for clinical research, and the PBMC quality is critical in obtaining accurate and reliable research results. Several quality factors need consideration during the isolation process, including sample collection, processing, counting, viability, and cryopreservation. Clinical research institutions must adhere to stringent quality controls during PBMC isolation to ensure that the isolated PBMCs are of high quality and suitable for research. By prioritizing PBMC quality control measures, researchers can ensure that the outcomes of their studies are both accurate and reliable.



Share On: